Vascularized Lymph node transfer (VLNT) for Lymphoedema: Is it possible and works?
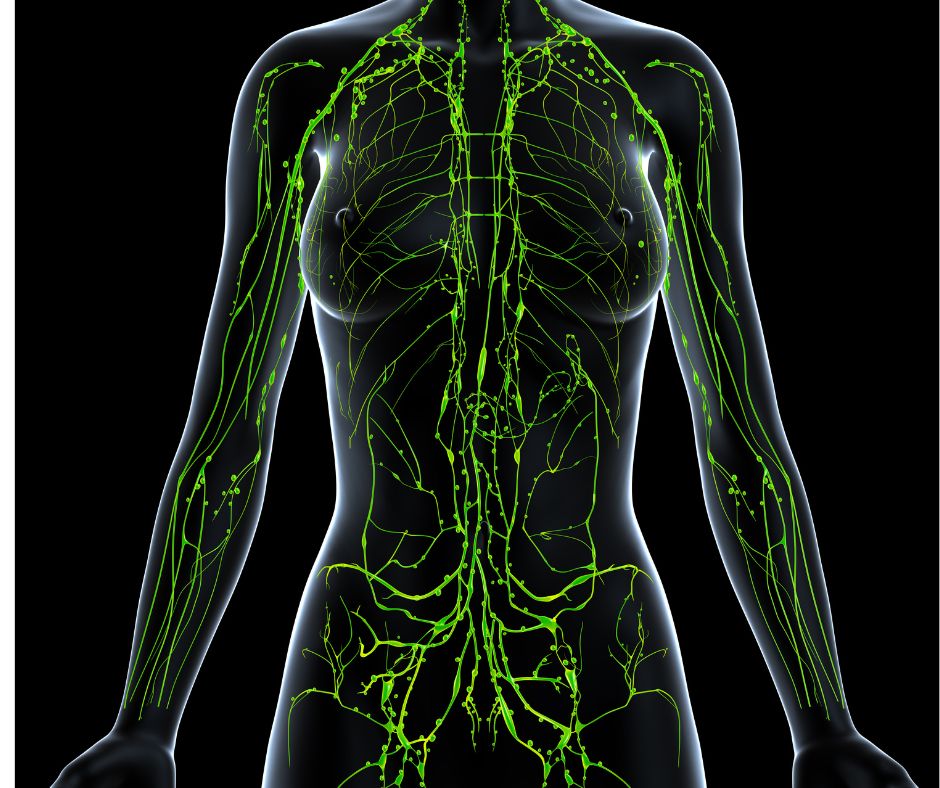
Persistent swelling? Lymphoedema is a chronic swelling condition, most seen in legs, arms or the nearest area where there is a lymphatic system dysfunction. It´s mainly caused by lymph node removal or damage during cancer treatments or other types of surgeries; trauma or genetic. Lymphoedema treatment is based on hands-on treatments and lifestyle changes. But in recent years, surgeons have been performing what seems to be a promising surgical solution. It is lymph node transfer surgery, also known as vascularized lymph node transfer (VLNT) for lymphoedema. A surgical option that offers hope for many patients who thought their condition was irreversible. By now, you may wonder: Is it possible and works? Let’s have a closer look…
What is Vascularised Lymph Node Transfer (VLNT)?
Vascularised lymph node transfer (VLNT) is a microsurgical procedure performed by experienced surgeons who harvest healthy lymph nodes (from a donor site e.g. groin, abdomen, or neck) complete with their blood vessels, and transplant them into the area of the limb affected by lymphoedema. By connecting these nodes to local blood vessels, surgeons create new pathways for lymphatic fluid to drain, thereby restoring a more functional lymphatic operation.
Vascularised Lymph Node Transfer (VLNT) for Lymphoedema: How does it work?
The process involves the following steps:
- Donor site selection. Surgeons choose the best area with surplus (extra) lymph nodes; in order to minimize the risk of causing lymphedema at the donor site.
- They use reverse lymphatic mapping and imaging as help to ensure safety.
- Lymphatic nodes are harvested with their blood vessels.
- Transplantation. Specialised surgeons transplant, meticulously, the nodes and reconnect them to blood vessels using microscopes and fine sutures.
- Lymphangiogenesis. During the following weeks and months, the transplanted nodes encourage lymphangiogenesis, the growth of new lymphatic vessels, which can connect to the local circulation and start rerouting lymph fluid effectively to the nearest nodes. Here is where magic happens!
What does science say about VLNT?
Recent studies made in 89 patients – 88 female and 1 male-with different types of cancer (65 breast, 18 gynecologic, 2 melanoma and 4 other types of cancer) reported:
- Limb volume (swelling) reduction. The first year, limb volume reduced 8%, and the second year, it reduced 20%-28% or more.
- Less symptoms. Patients reported less swelling, heaviness, pain, and risk of complications such as cellulitis (skin infections).
- Improved life quality. Many patients can reduce daily compression garments after successful surgery. It has to be always advised and supervised by their lymphoedema team (surgeon, lymphoedema therapist, etc.).
- Restore immune function. The transplanted nodes help regain immune surveillance in the affected limb. In other words, restore lymphatic function to the area, reducing the frequency of infections.
Vascularized lymph node for lymphoedema: Is it safe?
Yes, it is. The reverse lymphatic mapping reduces the risk of developing lymphoedema at the donor site.
Are there any risk factors?
As with any surgery, risks include infection, scarring, or failure of the harvest nodes to survive However, major complications are rare, for that reason your surgery should be performed by experienced microsurgeons.
Are there any side effects?
A case study of 89 patients after VLNT 14 reported complications like:
- 1 hernia in the donor site
- 1 episode of transient pancreatitis (pancreas inflammation-treated with medicines)
- 2 cases of flap loss (transplanted piece of tissue loss )
- 1 case of partial flap loss (just part of the tissue is lost)
- 3 reported hematoma
- 3 reported seroma
- 2 postoperative infection
- 1 wound dehiscence (wound open/tissue separation)
Vascularized Lymph Node for Lymphoedema:Are there more studies or trials?
Yes, there are, here some key Clinical Studies and Trials
1. Randomized Controlled Trial – Stage II Breast Cancer–Related Lymphedema
- 36 women randomized: 18 underwent VLNT + physiotherapy/compression, and 18 had conservative therapy only
- After 18 months: VLNT group had an average 57% volume reduction vs 18% in control
- Infection episodes dropped significantly in VLNT group
- Functional improvements and reduced heaviness/pain were reported
- VLNT found to be more cost‑effective than conservative care alone
2. Large Prospective Series – Combined VLNT & Lymphovenous Bypass (LVB)
- 328 patients treated; 67% underwent VLNT + LVB
- Avg volume reductions: 21.4% at 1 year, 36.2% at 2 years, with sustained benefits up to 4 years
- Quality-of-life scores (Lymphedema Life Impact Scale) improved significantly over time
3. Suction-Assisted Lipectomy (SAL) + VLNT
- 94 patients with stage IIb–III lymphedema
- Over ~3 years follow‑up: 60% reduction in lower-limb circumference and up to 81% in upper limb at various levels
- Cellulitis episodes were significantly reduced
4. Lymph Node Flap Transfer for Lower Limb Lymphedema
- Retrospective review of 52 cases: average 46.3% volume reduction in unilateral mild-to-moderate cases
- Better outcomes seen in less advanced presentations
5. Safety & Complications – Autologous Lymph Node Transplant (ALNT)
- Study of 26 patients (upper and lower limb): 38% had donor-site complications, including chronic lymphedema, lymphocele, pain
- Highlights need for careful patient selection and surgical technique
6. Emerging Techniques – VLNT + Nanofibrillar Collagen Scaffolds (NCS)
- Observational comparison: VLNT alone vs VLNT combined with BioBridge® NCS
- Early results suggest enhanced lymphangiogenesis and longer-lasting drainage pathways with the scaffold-assisted method
How long is the recovery process?
Most patients stay in the hospital for several days or as suggested by their surgeons.
When can I see the results?
- Studies and clinical follow ups showed that most patients see full benefits of surgery up to two years afterwards.
- Remember that regular follow-up, physiotherapy (with your lymphoedema therapist), compression therapy, exercise, proper hydration and nutrition are essential during the recovery process and maintenance.
Who is a good candidate for VLNT or similar surgeries? When can I consider VLNT or similar surgeries?
- This surgery is most effective for people with secondary lymphedema (often due to cancer treatments)
- Patients who have not found lasting relief from conservative therapies.
- Lymphoedema carriers who get into an agreement with their surgeon and see VLNT or similar as the best treatment option.
To keep in mind: careful assessment and imaging guide patient selection (to see if you have donor sites or which one is the best for harvesting). These procedures are what ensure the best possible outcomes.
A final word
Vascularised lymph node transfer represents a new hope in the approach of lymphedema treatment and management. As it directly addresses the underlying lymphatic failure, it offers not just symptom relief but the opportunity for real, lasting results. Remember that the surgery by itself cannot do all the work, you should keep exercising, eating and hydrating properly, doing manual lymphatic drainage; and all together will give you long-lasting relief, improve your quality of life and, why not?, making you free from daily compression and discomfort.
We hope this information is useful for you. If you need advice or have any questions about our treatments, please contact us. You can find us in Mill Hill Broadway and Islington. We are always happy to help. If you like this blog, please share!
References:
https://pubmed.ncbi.nlm.nih.gov/25285683/
https://pmc.ncbi.nlm.nih.gov/articles/PMC9463125/
https://pmc.ncbi.nlm.nih.gov/articles/PMC4066306/
https://www.youtube.com/watch?v=TLKlMmjruaA
https://pubmed.ncbi.nlm.nih.gov/34994481/